This course is an edited transcript from the live course presented by Chris Wilson, PT, DSCPT, DPT, GCS. Please follow along with the course handout.
Learning Outcomes
- The participant will be able to describe at least three advances in the management of the patient with cancer and the rehabilitation implications.
- The participant will be able to describe at least three ways the multidisciplinary team is incorporated into rehabilitation services, in the cancer continuum of care.
- The participant will be able to list at least three modifications to the evaluation and at least three modifications to the interventions based on the patient's medical conditions.
- The participant will be able to outline at least three concepts related to exercise prescription that identifies rehab needs in the patient with cancer.
Cancer Rehabilitation Core Concepts
Nationwide, the area of cancer rehabilitation is growing. The purpose of this seminar is to start a conversation about cancer rehabilitation and what it means to the physical therapist and physical therapist assistant.
Statistics
- 1.68 million people were diagnosed with cancer in 2016
- 14.5 million individuals are currently living with cancer diagnosis (considered "cancer survivors")
- 41% of people in the United States will be diagnosed with cancer at some point in their lifetime
- Overall survivals from 2012 to 2018 was greater than 65%
- Women have a 1 in 3 chance of developing cancer in their lifetime; men have a 1 in 2 likelihood
- In 2016, 595,690 people died of cancer = 1,630 cancer deaths/day
- Cancer is the second most common cause of death in the U.S.., followed by cardiopulmonary disorders
- By 2030, cancer will surpass cardiopulmonary disorders as the major cause of death in the U.S.
If there is a positive side to cancer becoming the number one cause of death, it is that it is going to get a lot more attention (e.g., research, treatment, prevention, rehabilitation, etc.). Physical therapists have to position themselves as the provider of choice when it comes to helping to rehabilitate these individuals as they go through their cancer survivorship journey.
Common Types of Cancer
First, we will look at the estimated new cases of cancer among men and women, as reported by the American Cancer Society (2015). In men, the type of cancer estimated to have the newest cases is prostate cancer. In females, there are more new cases of breast cancer than any other type. In both men and women, lung/bronchus cancer ranks as having the second most new cases.
Next, we will look at which types of cancer cause the most deaths. Although lung/bronchus cancer accounts for the second most new cases of cancer, it is the number one cause of death in both males and females. For both males and females, the third most common cause of new cancer cases, as well as cancer that causes the third most deaths, is colon and rectal cancer. The number four cause of death for both sexes is pancreatic cancer. It's not a very frequently seen cancer, but when it is, unfortunately, it's very difficult to treat, and therefore the cause of death from pancreatic cancer is fairly high.
Age-Adjusted Cancer Death Rates: Men and Women
According to the American Cancer Society's most current data (2012), male deaths from lung and bronchus cancer in the 1990's were extremely high. In response, a lot of smoking cessation interventions and programs started to become more prevalent and raised awareness about the dangers of smoking. Since then, the lung cancer death rate has declined. The death rate for prostate cancer was also fairly high in the 1990's but has been declining over the last several years. Similarly, male colon and rectum cancer deaths are also trending downward. Unfortunately, in the case of pancreatic cancer, which is difficult to screen for and detect, the male death rate has remained relatively stable.
Among women, lung and bronchus cancer was an "equal opportunity" disease, as smoking increased among women during the 1960s and '70s. As a result, female lung cancer deaths were also high in the 1990s, and are now trending downwards due to awareness and screening. Breast cancer deaths, as well as female colon and rectum cancer deaths, are also declining. Unfortunately, the death rate due to pancreatic cancer remains stable among women.
Cancer Pathology and Terminology
When working with a cancer patient, most physical therapists already possess the required hands-on skills, and the exercise and treatment skills, as they are very similar to the treatments and exercises that we perform with our non-cancer patients. Odds are, for the most part, you as a clinician already have all the tools in your toolbox that you need to treat a cancer patient. The one exception may be if you are not a lymphedema therapist because a lot of these patients do require lymphedema treatment. Other than that, most of the interventions that you know will be applicable to the cancer pathology. With cancer patients, you will need to ask questions to determine what the patient has undergone, what conditions they might be experiencing, if there are any side effects of their treatments, and what type of cancer might be requiring certain types of interventions.
Terminology that is useful to know on the topic of cancer includes:
- Tumor type
- Tumor size
- Lymph node status
- Hormone receptor status (e.g., with breast cancer, whether the cancer is receptive to estrogen, progesterone, androgens)
- Cellular grade
- Her 2/neu status (a receptor that, when the cancer is diagnosed, indicates the patient has a more aggressive type of cancer)
- Skin, lymphatic, vascular invasion
Tumor Pathology. At the top of Figure 1 is a diagram that represents normal cellular division. However, somewhere along the line, a genetic mutation occurs. The DNA becomes damaged through radiation, or from inflammatory responses, resulting in abnormal cellular reproduction. The abnormal cells start to grow. Even among the cellular replication of cancer cells, there are subdivisions among these cells and subsequent mutations down the line. You might have one cancer cell that is one genetic abnormality, which might subsequently mutate and be completely different than the initial cell.
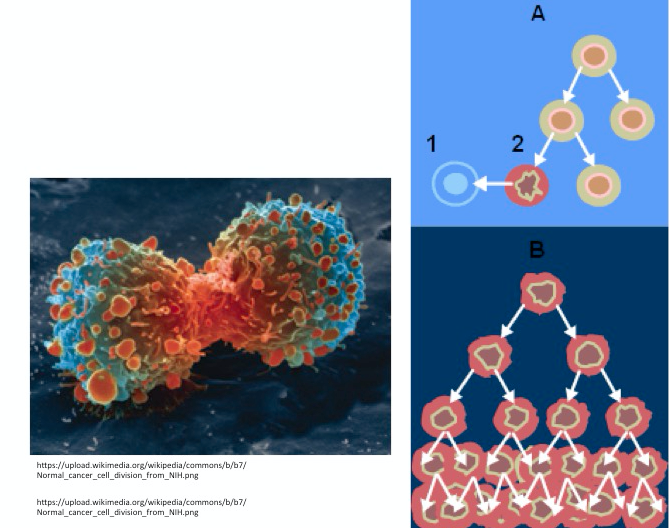
Figure 1. Cellular division and mutation.
There are two other terms that you are likely already familiar with, as they relate to cancer/tumors: benign and malignant. A benign tumor is simply a space occupying lesion. The bad news about benign tumors is that they can cause problems when they get bigger, and they can start to affect some of the normal cellular functions in the tissues around it. The good news is that if a tumor is benign, and it's resectable (i.e., the cancer can be cut out), theoretically, that the person will not have any more issues. Sometimes, they'll cut it out to the best of their ability, and then they'll do radiation to destroy any remaining cells that were in the area. The term malignant indicates that tumor has spread beyond its original location, usually through the lymphatic system to a distant site. We will go into this in further detail coming up shortly.
The average doubling time for the size of a tumor is about 200 days, for it to be a palpable tumor. As an example, if a patient was having a breast exam, for a tumor to be palpable, it has to be about one centimeter. However, the deeper the tumor is into the tissues, the harder it is for a person to palpate. Especially if the person doesn't have very skilled hands. As you probably all recall from physical therapy school, it took a little while for us to train our hands to be able to be sensitive enough to palpate. For a layperson to have that ability to palpate is fairly difficult. By the time a tumor is palpable, it's usually not a good sign. There are 50,000 to 100,000 genes per cell, and there are only 100 genes that are responsible for regulating cell growth.
Cancer Staging: TNM
There is a cancer staging system called TNM. It assesses tumors in three different capacities:
- T = Extent of the primary tumor
- N = Absence or presence of regional lymph node involvement
- M = Absence or presence of distant metastases
Using breast cancer as an example, the extent of the primary tumor would be the T. If there were lymph node involvement, that would be a positive N. Then, absence or presence of distant metastases would be the M. Every tumor has some type of grading system, or scaling system. It's beyond the scope of this class to explain in detail all of the different grading systems; just be aware that they exist.
Once T, N and M are determined, a stage of I, II, III or IV is assigned, with stage I being early stage and IV being advanced disease.
- Stage I is localized disease
- Stage II is axillary node involvement (affecting a few lymph nodes)
- Stage III is advanced regional disease without metastasis (multiple lymph node involvement)
- Stage IV involves distant metastases (it spread to a different part of their body or a different organ
Therefore, a case of breast cancer might be categorized as follows: T3N2M0. In other words, the extent of the primary tumor (T) is stage III; axillary node involvement (N) is positive and is stage II, and metastases (M) is not present (zero).
Metastatic Change
Here's how metastatic change works (Figure 2). You can see the tumor cells that are close to lymphatic tissue. They will start attaching to a lymphatic wall or a venous wall. This is when they start spreading to distant sites of lymph nodes. Finally, they'll become a secondary tumor, which is labeled a metastasis (also commonly abbreviated as a "met").
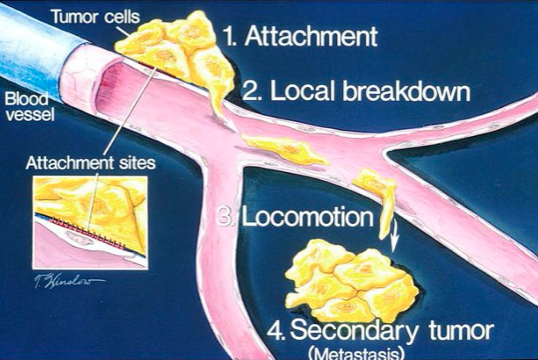
Figure 2. Illustration of metastatic change.
Bone Cancer
One of the things that physical therapists should be especially vigilant about is bone cancers. Figure 3 illustrates how bone cancer occurs and some of the common locations of bone cancers. As PTs, the primary areas that we're most concerned about are spinal metastases and long bone metastases. In the enlarged image on the left side of Figure 3, it shows where the lymph nodes settled cancer into a bone and caused a tumor at the neck of the humerus. If the patient were to fall while reaching out to stabilize him or herself, it could cause a pathologic fracture. This can also happen in the cases of spinal metastatic tumors. If the vertebral body is invaded with soft tissue, it can cause the vertebral body to collapse on itself, resulting in a pathologic compression fracture. Therapists should also be watchful of the femur because it's a weight-bearing bone, especially where there are transitions in forces. The neck of the femur is an area that if there was a metastatic lesion, I would have a conversation with my oncologist colleagues to obtain their advice on whether specific interventions might be harmful to a patient.
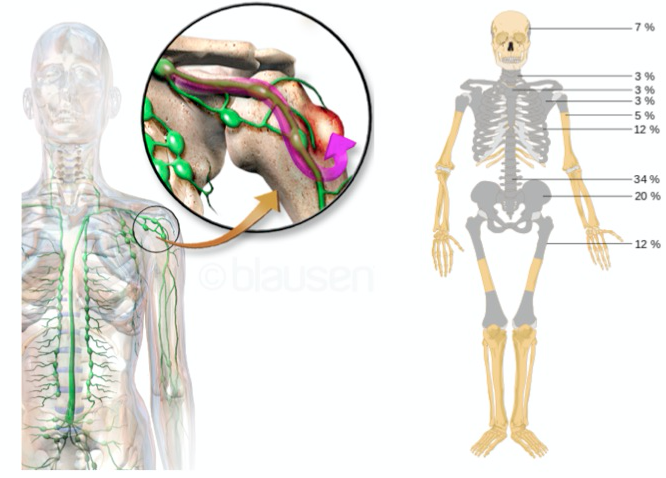
Figure 3. Bone metastasis average distribution.
Whenever you see or hear the word metastases, especially when you hear bone metastases, unless the patient has had a very recent visit with their oncologist, that would prompt me to call the oncologist and ask how much metastatic disease we are dealing with. If it's a small amount of disease, or it's widespread, but the tumors are extremely small, sometimes it doesn't require any modification to our treatment plan. If the tumors are relatively large (greater than 50% of the cortex), that might prompt us to be non-weight bearing.
Screening for Metastasis
Any cancer survivor should be monitored for metastatic disease. Even if you're not a cancer therapist, you will undoubtedly be seeing patients with a history of cancer. You need to keep an eye out for metastasis. Unfortunately, some of our patients who are cancer survivors and have been in remission or have been cured of cancer may have a recurrence of cancer. Furthermore, sometimes the initial symptoms of recurrence of cancer are from metastatic change. Examples of these symptoms in the brain may include headaches, seizures or vertigo. In the lungs, it could be a cough, hemoptysis (blood in the sputum) or dyspnea (shortness of breath). They might have lymphadenopathy, hepatomegaly (growth of the liver) or jaundice (yellowing of the skin). Again, if it is skeletal, they could experience pain, fractures, and spinal cord compressions.
Lymph Nodes
If lymph nodes are extremely tender and swollen but mobile, those are generally not signs of a cancer disease process. If they're hard and immobile and not necessarily super tender to the touch, a physical therapist might want to have a conversation with an oncologist or have the patient go in for a follow-up. Of course, that is a difficult conversation to have. I would caution all of you to tread into that conversation lightly. We don't want to alarm our patients, especially if they're cancer survivors. However, we do want to make sure that they're getting a routine checkup by their doctor. It might only require monitoring, but sometimes referral and workup are necessary. Sometimes if the patient has tenderness in the axillary area, or maybe has a swollen lymph node, you as a therapist might monitor that for a couple of days. If they come down with a cold, then you will know it was just an infectious disease process. If it's not necessarily changing, or it's growing without any type of signs of inflammation, like a fever or purulent drainage somewhere, or something that was related to an infection, that's a little bit more cause for concern. At that point, you might want to consult a physician, and they can talk to the patient about scheduling a follow-up visit.
Common Sites and Symptoms of Cancer Metastasis
There are relatively predictable locations where certain cancers will spread (Figure 4). This is useful information, especially when you're starting to work with a patient who might, for example, have lung cancer. Their disease process might spread to the adrenal glands, brain, and bone. If I have a patient with lung cancer, not only am I worried about their lungs and some of the difficulty with the cardiopulmonary system, I am also closely screening them for metastatic disease in the brain (e.g., confusion, disorientation, blurred vision, cognitive related changes). We also need to be cognizant of whether the patient has been recently screened for metastatic bone disease. Breast cancer commonly spreads to bone, liver, lung, and brain. Colon cancer will often spread to the liver. Pancreatic cancer may spread to the liver and lungs. Melanoma spreads mainly to the brain. Ovarian cancer may affect the pleural cavity and liver. Prostate cancer, of course, occurs only in males, often metastasizes to the bone. As a physical therapist, I am always concerned about brain mets and bone mets, because those are the body parts that I'm working with consistently. I want to make sure that they're not impaired.
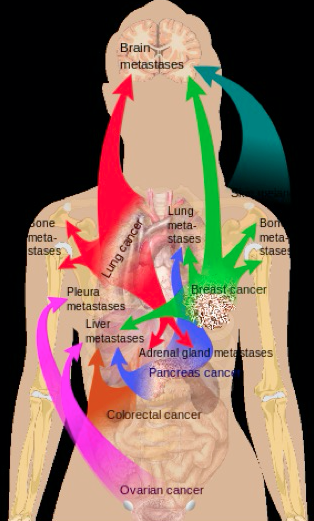
Figure 4. Common sites of metastatic change.
Cancer Treatments and Side Effects
As PTs and PTAs, when we work with patients who have had surgery, the same therapeutic principles apply. We want to optimize healing. We want to minimize scar tissue formation. We want to preserve range of motion and strength. However, we do need to realize that with this patient population, they might experience slower healing times. Due to suppressed immune systems, they might have increased risk of infections. There are two main categories of cancer treatment: local treatments and systemic treatments. Local treatments involve either surgery and/or radiation. Systemic treatments include hormone therapy, chemotherapy or other types of targeted medical therapies.
Chemotherapy
There are many different chemotherapy medications. Most are given by IV. For the purposes of today's presentation, we don't have enough time to go over all of them. We will highlight some of the types of chemotherapy, along with common side effects that you might see when you go to the clinic.
Adjuvant therapy is chemotherapy given to destroy any leftover microscopic cells that might be present after the known tumor is removed by the surgery. Adjuvant chemotherapy is usually given to prevent a tumor recurrence.
Neoadjuvant therapy is administered prior to the surgical procedure. The idea is that if the patient has to have surgery, it's much easier to deal with a small tumor than it is a larger tumor. The purpose of neoadjuvant therapy is to shrink cancer in order to give the surgeons the best chance of getting what we like to call "clean margins" (which I will define coming up shortly).
Induction chemotherapy is usually used to treat "wet" cancers. Wet cancers are usually blood-borne cancers, such as leukemia and lymphoma (as opposed to solid cancers, like lung cancer, breast cancer, and colon cancer). Induction is given to induce a remission in those leukemia or lymphoma type cancers.
Consolidation chemotherapy is given once a remission has been achieved. It is considered maintenance chemotherapy. The patient might need a low level of chemotherapy provided to them, potentially for the rest of their lives, to maintain that remission. Again, these are most commonly acute lymphocytic leukemias.
Palliative chemotherapy is specifically designed to address the symptoms of cancer. For example, palliative chemotherapy would be administered because a patient had a spinal cord tumor that was causing lower extremity paralysis. We are not going to cure that patient's metastatic disease in their spine. With a few very rare exceptions, when metastasis occurs, that cancer becomes a chronic condition that the patient will theoretically have for the rest of their lives. Palliative chemotherapy would shrink the tumor and decrease the pressure on the spinal cord. It is not curative, but just to reduce the symptoms to improve the quality of life.
Radiation
Radiation uses high-energy radioactive beams to kill cancer cells by damaging their DNA. This will shrink the tumor, and kill the cancer cells. There are different types of radiation, such as X-rays, gamma rays, charged particles (e.g., protons and electrons). One common misconception is that if someone undergoes radiation therapy, that they remain radioactive. This is untrue: as soon as the beam is turned off, they are not exposed to any more radiation. Furthermore, you will not be exposed to radiation if you are near someone who has received radiation therapy.
There are two different types of medications that are relatively new to radiation and cancer rehabilitation: radiosensitizers and radioprotectors. Radiosensitizers are drugs that make cancer cells more sensitive to the effects of the radiation therapy. There are a lot of agents that are under study as radiosensitizers. There are also radioprotectors. Radioprotectors are drugs that protect the normal cells from damage. The downside of radiation is that you are shooting a beam through an entire body part. If I had a tumor on my ulna, the radiation is going through my skin, my subcutaneous tissue, blood vessels, lymphatic vessels, my fascia, my muscles, finally to the ulna, and then back out through all of those other structures. Unfortunately for all of those structures, the tissue is also being damaged. As a result of radiation therapy, you can get frail skin, skin breakdown, scar tissue, and adhesions. The goal is to target only the tumor and leave those other tissues alone. That's why radioprotector medications are an exciting new area of study because those would hopefully promote repair of normal cells exposed to radiation, but leave the tumor cells highly vulnerable to the negative effects of the radiation.
Brachytherapy involves placement of a radioactive seed or pill in or near a tumor to slowly, over time, expose it to radiation, damage the cancerous tissues, and ultimately shrink the tumor. In this case, the patient may have a low level of radioactivity. There have not been any studies to prove that if someone was exposed to someone else's brachytherapy that they would have any negative effects. Be that as it may, there is still a low level of radiation.
Hormonal therapy includes some of those systemic therapies commonly used in breast and prostate cancer, which are more hormone-related cancers to slow the growth or prevent a recurrence.
Monitoring, or "watchful waiting" can be a controversial approach for cancer treatment. Admittedly, if I was diagnosed with cancer, and the doctor told me, "We're just going to wait and see what happens," I might not be too excited about that. However, studies are starting to show that in some cases of extremely slow-growing tumors, if we start doing aggressive chemotherapy and radiation and surgery, we might do more harm than good. Especially for older adults in their 80s or 90s, the treatments that we might use to cure their cancer might actually shorten their lifespan, as opposed to curing their cancer. Again, it's a little bit controversial. As a therapist, these are all things that are important to be aware of, because these are questions that we might get asked. Should I be doing watchful waiting? What do you think about that? Start thinking about that and get ready to have those conversations with your patients if you haven't already.
Types of Cancer
Next, we're going to discuss the top four types of cancer: lung, prostate, colorectal, and breast cancer. We will also cover some other cancer concepts.
Lung Cancer
Lung cancer is the second most commonly diagnosed type of cancer, but it's the leading cause of death. Unfortunately, because of lung cancer's symptoms of dyspnea and blood in the sputum, it's usually diagnosed at later stages (Stage III or Stage IV). It's difficult to screen for, and it frequently metastasizes to the brain.
There are a couple of different types of lung cancers. One type is called non-small cell lung cancer (NSCLC), which accounts for 80-85% of all cases. Small cell lung cancer (SCLC) accounts for 15-20% of cases. A bronchoscopy is a diagnostic procedure for determining whether someone has a certain stage of cancer, or whether they have cancer at all. They put a camera down the windpipe to determine the presence of cancer. Sometimes they can biopsy a suspicious nodule from a bronchoscopy. If the cancer is resectable, the surgeon may perform a lobectomy, where they will cut out an entire lobe of the tumor cell, or the entire lobe of the lung that encased the tumor. If the cancer was in multiple lobes of the lung, then they may cut out the entire lung (a pneumonectomy), and any associated lymph nodes, to make sure that the patient doesn't experience any metastatic spread. Sometimes they'll end up having radiation and chemotherapy in addition to the surgery.
As a physical therapist or assistant, when we work with patients who have had a large portion of the lung or an entire lung removed, that patient is going to have some significant cardiopulmonary or cardiovascular airway exchange. We're going to need to slowly but consistently start working on getting that residual lung tissue to adapt through closely monitored aerobic exercise.
Prostate Cancer
Prostate cancer is the most commonly diagnosed cancer in men, and it's the second leading cause of cancer death. A lot of men don't go in for prostate screening because it is not a pleasant procedure. The good news is that there is a blood test called prostate-specific antigen (PSA) screening. There are also digital rectal exams. Ideally, you should have both types of tests. Prostate cancer is a hormonal cancer and is often sensitive to androgen deprivation therapy. Sometimes, if they deprive male patients of testosterone or testosterone-type hormones, it can stabilize or potentially shrink the prostate tumor size. If you get screened early, you may not have to undergo prostate cancer surgery, where they scrape out or potentially even remove the prostate. Some of the side effects, from either a radical prostatectomy or a transurethral prostate excision, include either temporary or permanent urinary incontinence, scar tissue, erectile dysfunction, and pain upon urination.
There are different stages or grades of prostate cancer. The score for prostate cancer is called Gleason's. There are different types of Gleason's patterns. They will take several core biopsies by taking different tissues from different parts of the prostate, and then "grade" the tissue sample from one to five. The sum of two Gleason grades is the Gleason score. These scores help determine the chances of the cancer spreading. If you hear a Gleason score closer to 10, you will know that that's a very aggressive cancer. If it's a two or less, that is a less aggressive score. Gleason scores help to guide the type of treatment.
Colorectal Cancer
Colorectal cancer is the third most common cancer, but it is also the third leading cause of death. The good news is that colorectal cancer is very susceptible to screening. If the patient gets routine colonoscopies, flex sigs (flexible sigmoidoscopy) or other routine screening techniques, that can lead to very good early prevention. Sometimes, the doctor will conduct a colonoscopy with the camera, and if they see something that looks suspicious or pre-cancerous, they will immediately nip it out, cauterize it, and move on. They do send out the tissue to be screened, but if anything looks funny within that colon when they're doing the colonoscopy, they'll take it out right then and there.
If the patient does end up having colon cancer, there are some common surgical treatments that you might see. There would be a colon resection, where they would cut the colon in half, and remove the tumorous tissue. Often the patient will need to use a colostomy bag, maybe for the rest of their lives. In some cases, after months to years, they can reanastomose the colon back together. Not every patient can get an anastomosis. Sometimes it depends on the health of the patient and the health of both segments of the colon.
Again, as physical therapists treating patients who have had colon cancer, we need to use caution. If I'm gait training them with a gait belt, or doing something that requires a lot of core abdominal engagement, and they have a colostomy or have had colon cancer, I would be very careful not to tighten the gait belt right over the colostomy.
Breast Cancer
First, we'll review the breast anatomy (Figure 5). The healthy female breast is made of 12 to 20 sections called lobes. Each lobe is made up of many lobules, which is the gland that, in a lactating female, would produce the milk. Lobules are shown in purple. The ducts are the white channels that would deliver the milk in the lactating female to the nipple. As you can see there are muscles underneath, as well as fatty tissue. Then you have pec major, pec minor, the ribs. Within that, there is embedded a lymphatic supply.

Figure 5. Review of breast anatomy.
Breast cancer is the most commonly diagnosed cancer in women and is the second-leading cause of cancer deaths. There are more breast cancer survivors than any other kind of cancer. At Beaumont Health's outpatient facility, we have more physical therapy encounters with breast cancer patients than any other type of cancer patient. In the inpatient acute care setting, it is more of a general mix.
There are different types of breast cancer, which can be categorized into two types: invasive and non-invasive (Figure 6). Invasive ductal is also known as infiltrating ductal (IDC). This type accounts for about 70% of the different types of cancers. There are some different subtypes of invasive ductal breast cancer, including medullary, mucinous, or tubular. Those are terms that you might hear radiologists or oncologists use. Next, there is invasive lobular, also known as infiltrating lobular (ILC). This type of cancer affects the breast lobes, as opposed to invasive ductal, which affects the ducts. ILC makes up about 15% of breast cancers. There are two types of non-invasive breast cancers: ductal carcinoma in situ and lobular carcinoma in situ.
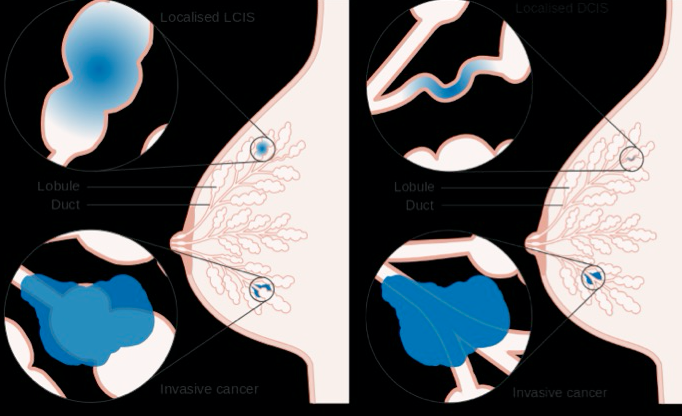
Figure 6. Invasive vs. non-invasive breast cancer (lobular and ductal).
The third type of invasive breast cancer is inflammatory breast cancer, which is generally very aggressive and difficult to treat. The overall prognosis for inflammatory breast cancer is not as great as with invasive ductal or lobular.
This diagram shows some of the different areas where cancers can appear (Figure 7). About 52% of breast cancers occur in multiple areas. In cases where the breast cancer is localized to a specific area, 25% of cases are found in the upper outer quadrant of the breast. If you are educating a patient on how to properly do breast self-exams, you definitely want them to pay attention to the upper outer quadrant of the breast, because that's where 1/4 of all of breast cancers are found. In some of the other areas of the breast, cancer occurs less often, although patients should be instructed to examine the entire breast. A smaller amount of cancers occur in the axillary tail of the breast, up along the line of pec major, pec minor area.
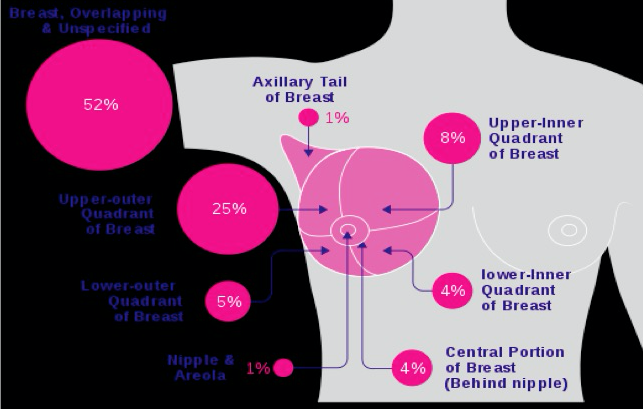
Figure 7. Common locations of breast cancer occurrences.
Figure 8 shows an example of a high-resolution mid-range infrared image depicting cancer in the right breast. In the left breast, you can see the thermal imaging is nice and purple. In the right breast, there are a couple of areas where you can see inflammation causing warmth, because of the increased vascularity of the breast tissue. This is not really a diagnostic image, but it hopefully gives you a good visual depiction of what some of the breast cancers might look like in relation to healthy breast tissue.
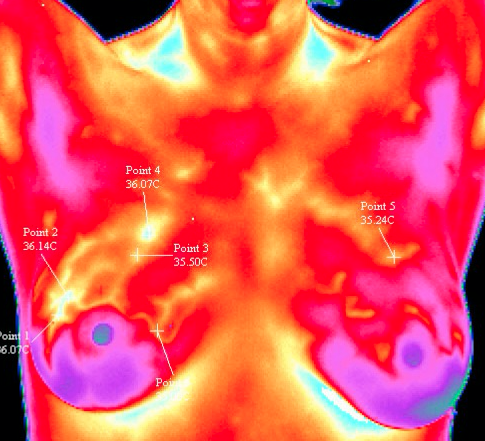
Figure 8. High-resolution infrared breast cancer image.
With inflammatory breast cancer, the breast becomes red and inflamed. Also, the texture of the skin becomes puckered, similar to the skin of an orange (i.e., "peau d'orange"). If you see that the skin on the breast is red, but textured like an orange, that might potentially be inflammatory breast cancer. Often, the nipple will also be inverted. Again, the prognosis for inflammatory breast cancer is not as good as other types of breast cancer.
Cancer as a Chronic Disease
Cancer is a chronic disease with long-term and late effects, especially for those with metastatic disease. As a therapist, working with cancer survivors, keep in mind that there are some immediate side effects that the patient will experience right after having been treated for cancer, but there are also late effects. Some patients experience cancer-related fatigue 10-20 years after they've had cancer. They might still have late stage onset of peripheral neuropathy. They might get numbness and tingling of their hands and feet from a chemotherapy that they had years ago. As such, we need to conduct appropriate screenings, and properly diagnose and treat musculoskeletal issues, cardiovascular and functional problems, as well as do our best to prevent and mitigate late effects.
Survivorship: Definition and Rationale for Rehab Services
The National Coalition for Cancer Survivorship (NCCS) pioneered the definition of a survivor as such:
- From the time of diagnosis and for the balance of life, a person diagnosed with cancer is a survivor.
- This expansive definition of "survivor" includes people who are dying from untreatable cancer.
- NCCS later expanded the definition of survivor even further to include family, friends and voluntary caregivers who are affected by the diagnosis in any way.
Additionally, the Association of Community Cancer Centers (ACCC) guidelines recommend health promotion and wellness:
Guideline I: Comprehensive rehabilitation services are available to cancer patients and their families through the entire cancer care continuum from diagnosis through survivorship.
Rationale: Cancer is a chronic disease that may require adjustment in the physical, social, financial and emotional aspects of life, in order to maximize independence and quality of life within medical status. Professionals experienced in rehabilitation are best suited to meet these needs of cancer patients.
If you are trying to start a new cancer rehabilitation program, or grow an existing one, you can present these definitions and guidelines from the NCCS and ACCC to hospital administration, to justify the need for cancer rehab services.
Chemotherapy Interventions
Chemotherapy is a systemic treatment, administered orally or via IV, used to kill rapidly dividing highly metabolic cells. This includes cancer cells, as well as normal cells, such as hair follicle, esophageal, stomach and blood cells. Chemotherapy drugs are considered to be cytotoxic (i.e, toxic to living cells). Many cancer patients lose their hair. Hair follicle preservation treatments exist that can be used during chemotherapy. This involves placing a cooling helmet on the patient's head to help to preserve hair.
Another important thing for a physical therapist to know is that when someone gets chemotherapy, they can potentially experience pancytopenia. This is a deficiency of all three cellular components of the blood: red cells, white cells, and platelets. If you are an outpatient therapist, and you are treating someone who is undergoing or has completed chemotherapy, you will need to modify your treatment plan accordingly. For example, you might be less aggressive with joint mobilizations until you verify that the patient has enough platelets. If you are too aggressive, the patient could potentially get a hemarthrosis that would not be able to be coagulated or clotted, because they don't have enough platelets to properly clot.
Chemotherapy Drugs
During chemotherapy, many different drugs are given together in a sequence, usually every two to three weeks. The drug combination is determined by a variety of factors: age, pathology, tumor size, lymph node status. Perhaps most importantly, it is determined by a patient's co-morbidities and performance status. This is where physical therapists can make a significant, life-changing impact on cancer survivors. If the patient is physically stronger, healthier, and has a good cardiovascular status, they can tolerate more chemotherapy and more radiation. Doctors can use a more aggressive protocol, which is more likely to be successful and save the patient's life. Therapists can do prehabilitation on newly diagnosed cancer patients by placing them on an aggressive exercise regimen to get their entire body as strong as possible including their heart, lungs, muscles and bones. If they are initially stronger, they can receive more aggressive chemotherapy and are more likely to be successful. That can also have a downstream effect of reducing recurrence rates because more aggressive chemotherapy and improved tolerance to all their radiation can lead to the ability to zap every single cell that had potentially turned into cancer. Physical therapy can have a big impact.
The following is a list of common chemotherapy drugs:
- Adriamycin (doxorubicin)
- Cytoxin (cyclophosphamide)
- Taxol (paclitaxel)
- Taxotere (docetaxel)
- Carboplatin
- Gemzar
- Xeloda
- Navelbine
- Epirubicin
Side Effects
Although necessary to kill cancer, chemotherapy poisons the entire body. This takes a physical toll on patients; as such, the number one side effect of cancer is fatigue, often referred to as cancer-related fatigue (CRF). As previously stated, chemotherapy can cause decreased white blood count and immunosuppression. If you're an acute care therapist, some of your patients might be on what's known as protective isolation (a range of practices used in hospitals to protect immunocompromised patients from infection or further infection). Additionally, they may be experiencing hair loss, nausea, vomiting, malnutrition. They may also acquire peripheral neuropathies, pulmonary fibrosis, and kidney dysfunction. Some patients will get cardiac arrhythmias. Due to chemotherapy affecting the nerves and their impulse transmission, patients might experience ataxia, balance dysfunction and weakness from their chemotherapy.
In addition to the physical ailments caused by chemotherapy, patients commonly experience mental fogginess, also known as chemobrain. This involves the inability to retrieve specific words, memory issues, similar to being sleep deprived and not "firing on all cylinders." Some cancer survivors are just happy to be alive, and accept that chemobrain is their new normal. However, this is a misconception. As physical therapists, we can help these people. There are techniques we can employ, such as exercise, that have been shown to help with cancer-related fatigue and chemobrain.
Tumor Heterogeneity
A tumor or cell in its early stages may begin as one specific tumor heterogeneity or one kind of genetic line. As it grows, when it reaches about the one-centimeter size and becomes a palpable tumor, the millions of cells that comprise the tumor have become distant relatives. Some of the tumor cells might have different medication sensitivities at different times. The medical oncologist may periodically switch tumor protocols. Certain medications that work for one specific tumor line, may not be effective with the other specific tumor line.
Cardiotoxicity
Certain chemotherapy drugs have the side effect of weakening and damaging the heart muscle. As physical therapists, we need to be familiar with these drugs. The most common drug is Adriamycin. If a therapy patient is using Adriamycin, we need to modify our treatment schedule to use less aggressive aerobic exercise, and to monitor them more closely. We need to take a detailed assessment of their rate of perceived exertion. Some of the expected symptoms of cardiotoxicity include dyspnea on exertion, a persistent cough, edema in their feet, or even difficulty with breathing. Sometimes the physicians will do a multi-gated acquisition (MUGA) scan to monitor the efficiency with which the heart pumps.
When rehabilitating a patient who has cardiotoxicity, begin with closely monitored, gentle strengthening aerobic assessments, using things like a treadmill or a stationary bike. If your patient has cardiotoxicity, you should definitely conduct a graded exercise test to determine their level of aerobic ability. Maybe a bike test, a Bruce protocol treadmill test or something to determine if your patient is cardiovascularly impaired. The good news for rehabilitation is that the procedures are very similar for patients who've had a myocardial infarction, or some other type of cardiovascular insult. We'll want to more closely monitor heart rate, blood pressure, and pulse oximetry. It is useful to use the Borg Rating of Perceived Exertion, so the patient can rate how exhausted they feel on a scale of 6-20. Then slowly and incrementally progress their exercises.
Bone and Muscle Loss
Some chemotherapy medications will cause bone loss (osteopenia and osteoporosis) and muscle wasting (sarcopenia). To counteract bone loss, we can use weight-bearing exercises, walking and weight lifting, progressive resistive exercises. We might even be able to do some of those in a preventative manner. Patients with muscle loss will also respond very well to resistive exercises and weight training.
Hearing Loss
Certain types of chemotherapy medications can cause ototoxicity or hearing loss. These are usually platinum-based medications. Very handily, they have named these drugs using the suffix "platin" at the end. If you see Cisplatin or Carboplatin, those are platinum-based chemotherapy medications. They might potentially cause dizziness, tinnitus, ringing in the ears, or even hearing loss. Some of our patients might experience dizziness, similar to benign positional vertigo disorders.
Targeted/Hormonal Therapies
Targeted/hormonal therapies are IV and oral medications, usually cytostatic, designed to change the hormonal or biological environment of the cancer cell to restrict its growth. They're not technically chemotherapy; they're more hormonal or biological agents that can be used as maintenance medications. As we talked about earlier with prostate cancer and breast cancer, estrogen or testosterone blockers are considered to be cytostatic (inhibiting cell growth). Herceptin is another one. Avastin or bisphosphonates are often used in the case of osteoporosis or osteopenia, as well as some of the cancer-related interventions.
Radiation Therapy
As stated earlier, radiation damages DNA in the nucleus of the cancer cell. Radiation is usually given in small doses over long periods of time. Just as surgery and chemotherapy cause fatigue, so does radiation. It can also cause reduced red and white blood cell counts, as well as low platelet counts. There are different tissue tolerances. The first time someone gets radiation, you might not necessarily see any skin changes. It's a cumulative effect. The more sessions of radiation that the patient gets, the more tissue changes you can expect to see. The acute tissue tolerance is one to four months (while undergoing treatment). Intermediately is up to four to 12 months. Finally, you can even have chronic tolerance issues or tissue changes up to eight years after the patient has had radiation therapy.
Treatment Planning
Before a person gets radiation, first they'll receive treatment planning. Usually, they will get CT scan images from what they call a simulation (Sim) and transfer them to planning software (Pinnacle). The physician will contour the actual tumor cell and try and focus just on those tumor cells while still trying to preserve the normal tissues. Next, they have very sophisticated algorithms to determine the prescription dose. Then they'll formulate a treatment plan. Finally, the physician approves the specific treatment plan for their radiation.
Prescribing Radiation
Conventional radiation therapy is dosed in units called Gray. The dose is selected based on the tumor type, location, and the goals of treatment (i.e., curative or palliative). They will divide the radiation into fractions, delivered daily until the total prescription dose is achieved. The duration of radiation therapy can last from two to eight weeks. There are standard radiation treatments, delivered daily (Monday through Friday). Then, there is Stereotactic Body Radiation Therapy (SBRT). These are higher-dose conformal treatments, delivered in one to five fractions every two to three days. SBRT is used for lung, spine, adrenal or brain cancer.
Radiation therapy is commonly used in/on the following locations:
- CNS: brain and spine
- Head & Neck
- Breast
- Lung
- GI: esophagus, gastric, pancreatic, biliary, colon, rectum, anus
- Gyn: cervical, uterine, vaginal, vulvar
- GU: prostate, bladder, testicular, urethral
- Sarcomas
- Skin cancers
- Pediatrics
- Bone metastases from any primary
Generally, if someone has to have a surgical resection, radiation is going to be considered if they're concerned about tumor margins or clean lines of cancer.
Immobilization
In order to receive their simulation and radiation treatment, patients need to be immobilized or held in one spot. If a patient cannot tolerate immobilization, they will be unable to receive the optimal dosage of the radiation. This may result in not being able to kill all the tumor cells, and potentially creating a higher risk of recurrence. This is where a PT or PTA can make a valuable contribution to the care team. For example, if the patient has an adhesive capsulitis and can't get their arm into a specific position, or maybe they have a herniated disc in their neck and they can't tolerate the appropriate position, they're not going to get effective treatment. Therefore, if we can fix those musculoskeletal dysfunctions, that can make a big difference in the patients being able to tolerate that radiation treatment. If a patient needs to undergo multiple sessions of radiation, sometimes they will receive a small tattoo or ink marks, whether permanent or temporary, on their body to help with subsequent set-ups.
There are many variations of immobilization. For the purposes of this course, we will look at examples of three different applications:
- Blue bag immobilization for an upper C-spine SBRT case (Figure 9)
- Head & Neck or Brain Aquaplast mask: used to immobilize the head and neck for one specific intervention (Figure 9)
- Breast immobilization: either the patient is supine with arms overhead, or prone to distract the targeted breast tissue away from the rib cage (Figure 10)
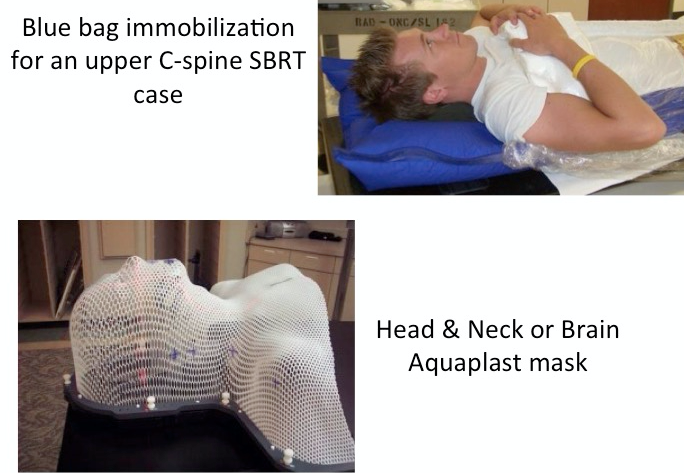
Figure 9. Types of immobilization.
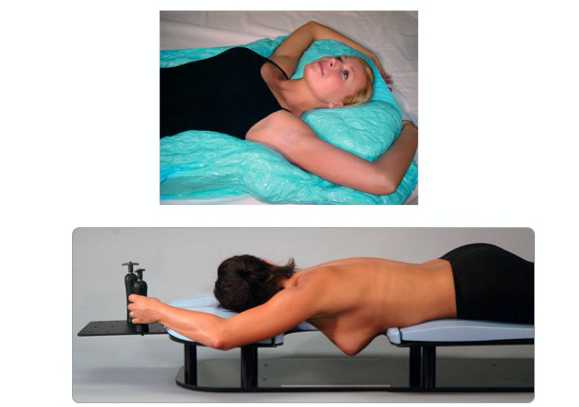
Figure 10. Breast immobilization.
Types of Radiation
One type of radiation uses a linear accelerator, which delivers external beam radiation therapy (EBRT) (Figure 11). Essentially, it's a photon (or X-ray) beam created outside of the patient in the treatment unit head, and then directed toward the patient at a variety of angles. The patient will not feel, hear, see or smell radiation that's being delivered. It ranges from a few minutes to 45 minutes, depending on the complexity of the plan and the site of the treatment.

Figure 11. Linear accelerator.
Figure 12 shows some examples of brachytherapy. Again, the term "brachy" means short distance. It's a delivery of radiation therapy via either interstitial or intracavitary implants over a short distance. This is radiation delivered from the inside out, as opposed to from the outside in. The source is either delivered permanently or temporarily, and is commonly used for prostate, breast, head and neck cancers, cervical cancers, uterine, or even ocular melanomas of the eye.
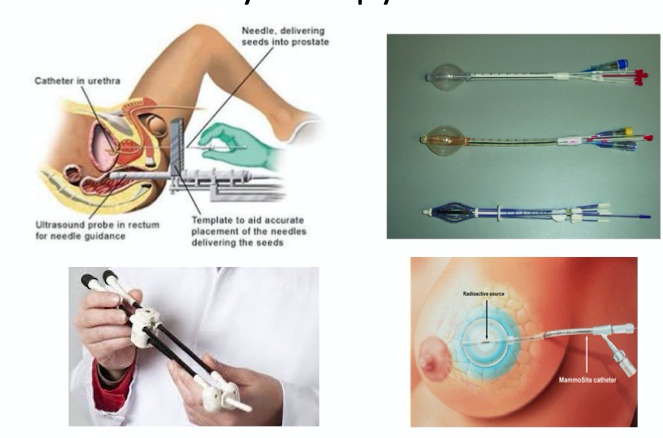
Figure 12. Brachytherapy devices.
Gamma knife is another commonly seen radiation delivery method (Figure 13). This is often used for the treatment of intracranial tumors. They use cobalt-60 radiation sources focused at a fixed point. It's highly conformal. It's very appropriately targeted to the cancer tissues while preserving brain tissues. Gamma knife uses a rigid stereotactic head frame in order to closely immobilize that body area to only target the affected brain tissues. This might be used if there is an area where the brain tissue is highly sensitive and we don't want to damage it.
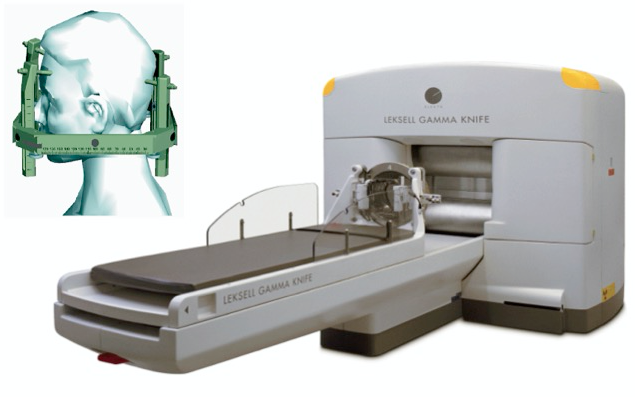
Figure 13. Gamma Knife Stereotactic Radiosurgery.
There's also proton therapy, which is external beam radiation delivered using protons as opposed to photons. One advantage of proton therapy is that protons have a finite range in tissue, and it can spare more normal tissue. The good news is that radiation treatment techniques are getting better and better targeted, so they have fewer side effects. When you hear gamma knife or proton, that usually means that you can expect less damage of healthy tissue.
Implications of Radiation
One of the implications of radiation includes desquamination, or cumulative burning of the skin. Additionally, these patients can experience mild to severe fatigue, as well as tissue fibrosis, from 6 to 36 months post radiation. This is an example of why physical therapists should have a long-term relationship with their cancer patients. We should be screening them periodically, because they might not develop tissue fibrosis changes until six months or more after their treatment has stopped. They might need to be on a preventative range of motion schedule. If they start losing range of motion, they need to call us to start working on some myofascial techniques to start working to break some of those adhesions or fibroses. Other effects of radiation include aggravated lymphedema and lymphatic cording which will increase lymphedema risk. Patients might even experience weakness at that site. If the patient does get radiation that goes over nerves, for example, like the brachial plexus, you might get some muscular weakness in a characteristic pattern for a brachial plexopathy. We should be screening for that as well.
Rehabilitation Needs
The needs of each patient are going to be driven by their specific symptoms, some of which include:
- Fatigue
- Weakness or numbness
- Poor endurance
- Balance or postural changes
- Joint stiffness
- Pain
- Difficulty with restriction ambulation
- Scar tissue
- Lymphedema
- Decreased range of motion
The good news is that as therapists, these are all issues that we're already experienced in treating. It is critical that we have access to these patients so that we can get to them early and often.
Acute and Late Stage Radiation Toxicity
Toxicities are highly dependent on the body or the tumor site being treated. The acute toxicities are going to be managed through the treatment course, but late toxicity needs to be assessed at follow-up visits, and definitely, can require referral to physical and occupational therapy. If you're working with your patients in the early stage, hopefully, you will let them know about some of those late effects (e.g., cording, lymphedema, radiation fibrosis). If they start losing range of motion or having pain or dysfunction, you can work with them to return to the therapy clinic.
Acute Side Effects
We have broken down the acute side effects of radiation by location and system: brain, head and neck, breast, GI/GU/Gyn, and lung/bone/sarcoma. Fatigue is a common symptom across all of these areas. The good news is that PTs and PTAs can play an important role in mitigating fatigue with exercise.
Brain. Acutely, if the patient has had recently radiation on the brain, they might experience the following acute side effects:
- Fatigue
- Alopecia
- Scalp itching/irritation/skin changes
- Nausea/vomiting
- Headaches
- Balance difficulties
- Other focal central nervous system findings
Head/Neck. Head and neck cancer patients will certainly have fatigue, along with other side effects, such as:
- Skin changes in the treatment field – erythema, hyperpigmentation, itching, dryness
- Nausea/vomiting/changes in bowel habits
- Weakness, difficulty with ambulation
- Back pain
Breast. With regard to breast cancer, almost every lumpectomy will require some type of radiation. It's also done for some mastectomies. They may radiate the entire chest wall. Sometimes they will preserve axillary and supraclavicular nodes. If there are four or more positive lymph nodes, they might provide more specific radiation, or even excise those. Acute side effects of breast cancer radiation include:
- Skin reaction – erythema, hyperpigmentation, itching, desquamation
- Breast or arm swelling
- Decreased range of arm motion (due to fibrosis)
- Tightness in the axilla/chest wall
- Fatigue
Just like with any other patient that has undergone an acute surgery, we want to increase the flexibility of the axilla/chest wall area, but not overstretch them to such a degree where we damage the tissues. Use exercises that are within their comfort level for stretching and range of motion, as opposed to aggressive manual stretching.
GI/GU/Gyn. If the patient has had GI/GU/Gyn radiation, here are some of the different acute side effects that you can expect:
- GI: Nausea, vomiting, abdominal pain, decreased appetite, diarrhea, rectal discomfort, skin changes, bloating, fatigue
- GU: Dysuria, frequency, nocturia, diarrhea, rectal discomfort, fatigue
- Gyn: Dysuria, frequency, vaginal discomfort, diarrhea, skin changes, fatigue
Physical therapists working in outpatient settings traditionally do not often see GI/GU/Gyn patients. If any of you or your colleagues are pelvic floor therapists, you should make an effort to focus your practice also on genital, urinary, and Gyn cancers, because of the above symptoms.
Lung/Bone/Sarcoma. Some common side effects of lung, bone and sarcoma radiation include:
- Lung: Shortness of breath, chest discomfort, cough, esophagitis, dysphagia, skin changes, fatigue
- Bone Metastases: Pain, bone fractures, fatigue
- Sarcomas (extremities): Swelling, pain, skin changes, decreased range of motion, fatigue
Movement Disorders and PT After Radiation
Some movement disorders that can occur after radiation include:
- Decreased ROM
- Delayed pain
- Delayed breast swelling
- Delayed soft tissue dysfunction
- Decreased strength
- Fatigue
In Figure 14, you can see under the axilla of this patient, a lot of extremely tight tissues, along with some hyperpigmentation. We're going to have to do some consistent myofascial release or soft tissue mobilization with this patient, to restore that tissue fiber to its normal mobility.

Figure 14. Tight tissues as a result of radiation.
Physical therapy interventions after radiation include a flexibility and range of motion program, stretching, manual therapy, working on strength. We also want to include aerobic exercise, to help alleviate fatigue. Furthermore, we need to address any upcoming treatments, to keep the patient as strong and as flexible as possible, to mitigate future issues related to range of motion and tissue mobility, and to maximize the patient'
